What is Cholangiocarcinoma?
(Cholangiocarcinoma is pronounced kol-an-gee-oh-car-sin-oh-ma).
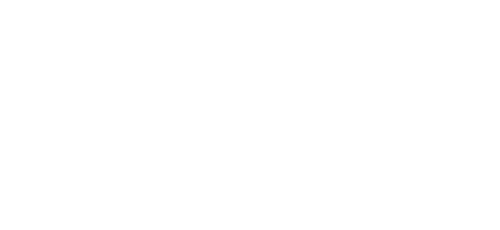
Cholangiocarcinoma (CCA), or bile duct cancer, is a primary liver cancer which starts in the inside lining of the ducts of the biliary tree; this is a network of tubes that carry bile from the liver to the gut. Depending on which part of the bile duct CCA develops in, it is categorised as one of three types:
- Intrahepatic CCA originates in the bile ducts within the liver
- Hilar or perihilar CCA originates just outside the liver, where the left and right hepatic ducts join together
- Extrahepatic or distal CCA originates in the common bile duct from just below the cystic duct, which joins the common bile duct and the gall bladder, down to the small intestine. The common bile duct carries bile from the liver and the gall bladder to the small intestine
Adenocarcinoma, cancer arising from the mucus glands lining the inside of the bile ducts, is the most common type of cholangiocarcinoma, accounting for up to 95% of all cases.
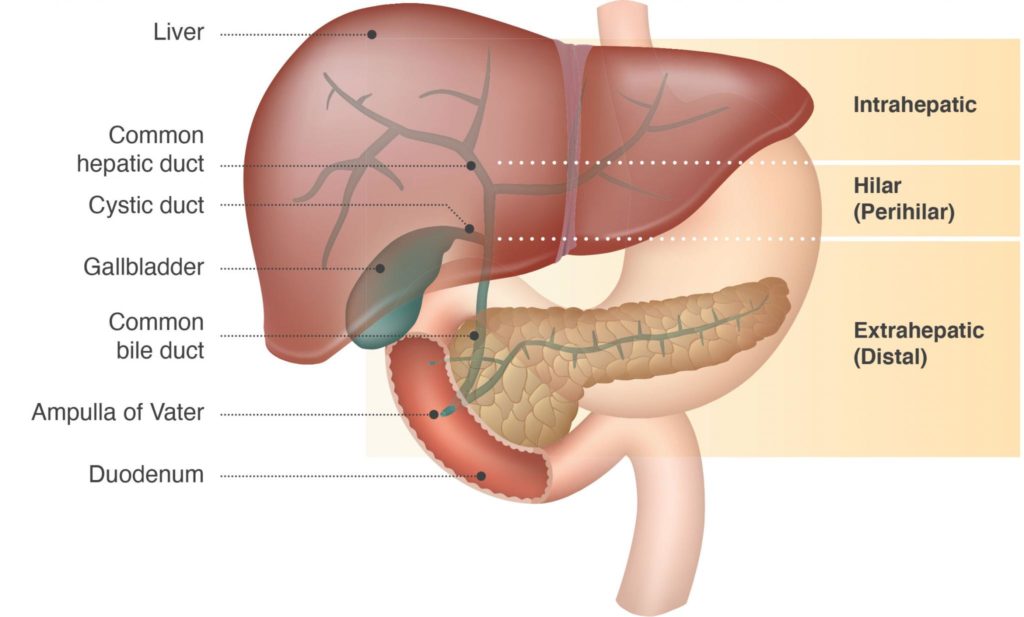
Illustration © AMMF 2023
Cholangiocarcinoma, also known as bile duct cancer, is a biliary tract cancer. The other biliary tract cancers are gallbladder cancer and ampullary (or ampulla of Vater) cancer:
Download the Biliary Tract Cancer Guide for Patients
Gallbladder cancer, a biliary tract cancer, originates in the cells of the gallbladder. Most are adenocarcinomas, which begin in the gland cells of the gallbladder lining. Symptoms are similar to CCA, but can also include nausea, and abdominal pain. More information on gallbladder cancer can be found in the Biliary Tract Cancer Guide for Patients, available as a download by clicking here
Ampullary cancer (or ampulla of Vater cancer) is the rarest of the biliary tract cancers. This develops where bile ducts from the liver and pancreas join and enter the duodenum in an area known as the ampulla of Vater. More information on ampullary cancer can be found in the Biliary Tract Cancer Guide for Patients, available as a download by clicking here
The biliary system explained
The biliary system includes the network, or tree-like structure, of ducts within the liver and the common bile duct outside the liver.
Within the liver the smaller ducts, similar to capillaries, drain bile1 from the cells of the liver into larger and larger branches. The right and left hepatic bile ducts inside the liver collect the bile, and join outside the liver to form the common bile duct (extrahepatic bile duct), which carries the bile from the liver to the gall bladder and down to the small intestine.
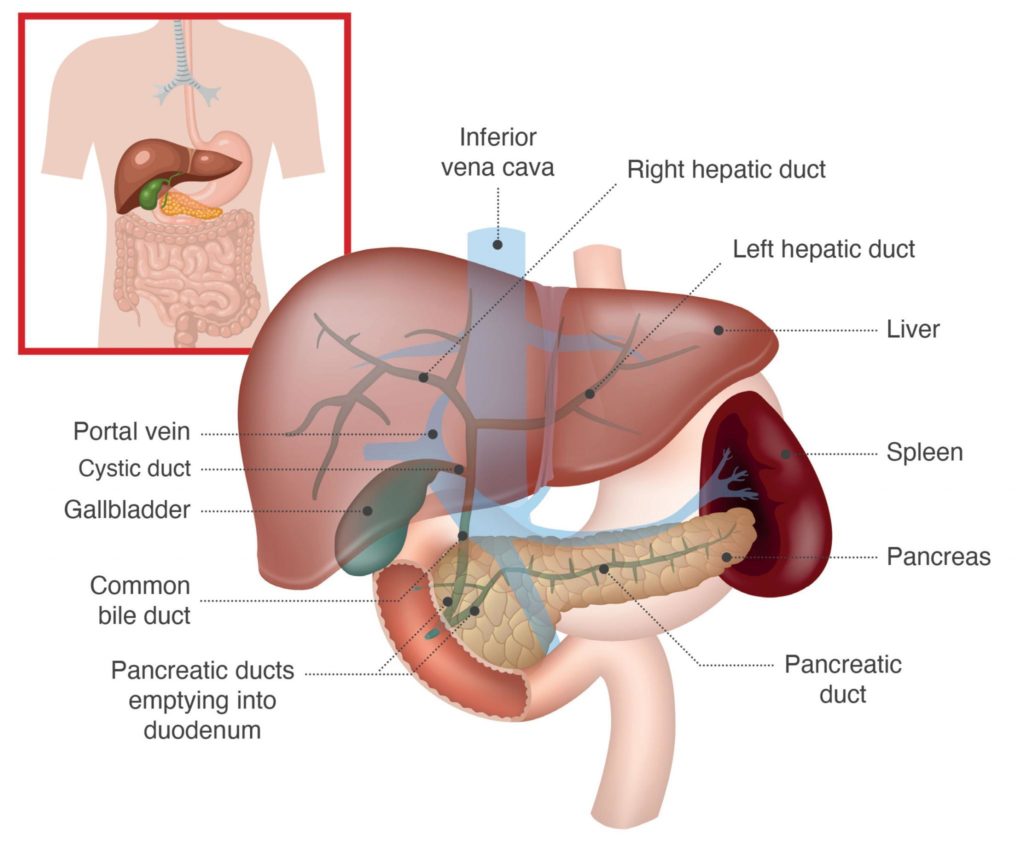
Illustration © AMMF 2023
The gallbladder acts as a reservoir to hold bile until food reaches the small intestine. It is attached by a small duct, called the cystic duct, to the common bile duct about one-third of the way down the common bile duct from the liver.
Where is the liver, and what does it do?
The liver is found just below the right lung and is protected from injury by the lower ribs. It is one of the most complex organs in the body. It acts like a “chemical factory” as it performs hundreds of tasks that are needed to keep the body healthy and alive, including:
- Fighting infection and disease
- Removing poisons and drugs (including alcohol)
- Cleaning the blood
- Controlling the amount of cholesterol
- Storing vitamins, minerals and sugar
- Processing food once it has been digested
- Helping to control blood clotting (thickening)
- Releasing bile1, the liquid that breaks down fats and helps digestion
1Bile is made in the liver and stored in the gallbladder. It helps to break down fats found in foods, and to rid the body of waste material filtered out of the bloodstream by the liver.
To download a copy of AMMF’s brochure, click here